Is Hypoglycemia a Sign of Diabetes?
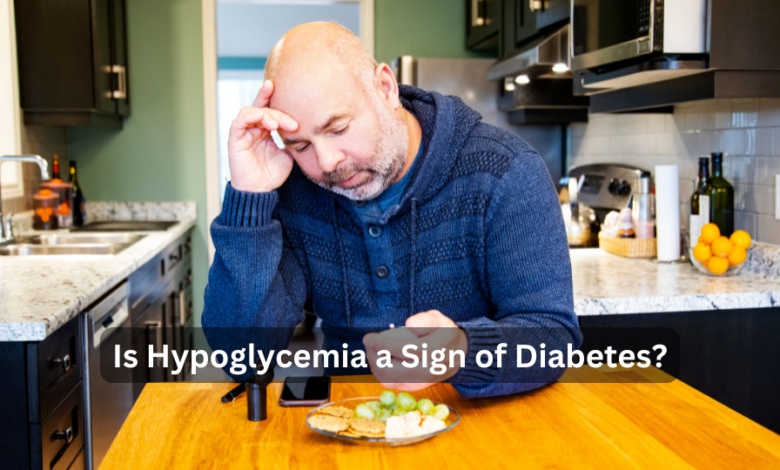
Hypoglycemia, or low blood sugar, is a condition that occurs when blood glucose levels drop below the normal range. While many associate diabetes with hyperglycemia (high blood sugar), hypoglycemia can also be closely linked to diabetes, particularly in those who are managing the condition. In this article, we will explore the connection between hypoglycemia and diabetes, the causes, symptoms, prevention, and treatment options. Understanding the complex relationship between hypoglycemia and diabetes can help individuals manage their health more effectively.
What is Hypoglycemia?
Hypoglycemia occurs when blood sugar levels fall below 70 mg/dL. While glucose is the body’s primary source of energy, particularly for the brain, insufficient glucose levels can lead to a range of symptoms that can affect daily functioning and overall health. Hypoglycemia can be a temporary issue or a chronic problem depending on its cause and the individual’s health condition.
Symptoms of Hypoglycemia
Recognizing the symptoms of hypoglycemia is crucial for timely intervention. Some common symptoms include:
- Shakiness
- Sweating
- Confusion or dizziness
- Hunger
- Rapid heartbeat
- Headache
- Irritability
In severe cases, hypoglycemia can lead to loss of consciousness, seizures, and even coma if left untreated. Immediate action is necessary when these symptoms are detected.
Is Hypoglycemia a Sign of Diabetes?
Hypoglycemia itself is not a standalone diagnosis for diabetes, but it is often a sign of poorly managed diabetes, particularly in individuals who are using insulin or other diabetes medications. For individuals with Type 1 diabetes and some with Type 2 diabetes, managing blood sugar levels can be a delicate balancing act. Medications, including insulin, are designed to lower blood sugar, but if the dosage or timing is incorrect, it can lead to dangerously low levels of glucose in the bloodstream.
Types of Diabetes and Hypoglycemia
- Type 1 Diabetes: This form of diabetes is characterized by the body’s inability to produce insulin, a hormone required to regulate blood sugar. Individuals with Type 1 diabetes rely on insulin therapy. Hypoglycemia can occur when there is an imbalance between insulin administration and food intake, or during periods of increased physical activity.
- Type 2 Diabetes: While Type 2 diabetes is more often associated with high blood sugar levels, hypoglycemia can also occur in individuals who take insulin or other blood sugar-lowering medications. Those on sulfonylureas or meglitinides are particularly at risk for hypoglycemia if they skip meals, exercise more than usual, or take too much medication.
- Gestational Diabetes: Hypoglycemia can also affect pregnant women with gestational diabetes, though it is less common than in Type 1 or Type 2 diabetes. Women managing gestational diabetes should monitor their blood sugar closely to avoid both hyperglycemia and hypoglycemia.
Causes of Hypoglycemia in Diabetics
There are several factors that contribute to the onset of hypoglycemia in individuals with diabetes. Understanding these triggers can help in better management:
Excessive Use of Insulin or Oral Medications
For those managing diabetes with insulin injections or oral antidiabetic medications, hypoglycemia often results from overmedication. Misjudging the correct dose of insulin, especially when combined with factors like reduced food intake or increased physical activity, can lead to a drop in blood sugar levels.
Inadequate Food Intake
Skipping meals or not eating enough carbohydrates is another common cause. Individuals with diabetes who skip meals while continuing to take their prescribed insulin or oral medications risk lowering their blood sugar to dangerous levels. Carbohydrates play a crucial role in maintaining blood glucose levels, and an imbalance between insulin and food can trigger hypoglycemia.
Excessive Physical Activity
Exercise helps to lower blood glucose, which is generally beneficial for people with diabetes. However, prolonged or intense physical activity can cause an excessive reduction in glucose levels, leading to hypoglycemia. People with diabetes need to adjust their medication and food intake according to their physical activity levels to avoid this risk.
Alcohol Consumption
Alcohol can interfere with the liver’s ability to release glucose into the bloodstream, especially when consumed on an empty stomach. This makes hypoglycemia more likely in individuals with diabetes who drink alcohol without eating a balanced meal beforehand. It’s recommended that individuals with diabetes who consume alcohol monitor their blood sugar levels closely.
Delayed or Missed Meals
When meals are delayed or missed, there is a lack of glucose intake to maintain stable blood sugar levels. If someone continues to take insulin or other blood sugar-lowering medications without consuming food, they risk hypoglycemia.
Hypoglycemia Unawareness
In some cases, people with diabetes may develop a condition known as hypoglycemia unawareness, where they are unable to recognize the early warning signs of low blood sugar. This condition is particularly dangerous because it can lead to severe hypoglycemia without the person realizing they need to take corrective action. Hypoglycemia unawareness occurs more frequently in individuals with Type 1 diabetes or those who have experienced frequent episodes of low blood sugar.
How to Prevent Hypoglycemia Unawareness
To prevent this condition, people with diabetes are encouraged to:
- Monitor blood sugar levels frequently.
- Adjust medication based on the advice of a healthcare provider.
- Avoid skipping meals.
- Be cautious of alcohol consumption.
How to Manage Hypoglycemia
When hypoglycemia occurs, quick action is needed to restore normal blood sugar levels. The following are effective steps to manage an episode:
- Consume Fast-Acting Carbohydrates: The first step in treating hypoglycemia is to consume 15-20 grams of fast-acting carbohydrates. Foods like glucose tablets, fruit juice, regular soda, or hard candy can quickly raise blood sugar levels.
- Recheck Blood Sugar Levels: After 15 minutes, individuals should recheck their blood sugar levels. If levels remain below 70 mg/dL, an additional 15 grams of carbohydrates should be consumed.
- Follow-Up Meal: Once blood sugar levels have stabilized, it’s important to eat a small meal or snack that contains a mix of carbohydrates and protein to prevent another drop in blood sugar. A peanut butter sandwich, cheese and crackers, or yogurt are good options.
- Glucagon Injection: In severe cases, where an individual is unconscious or unable to consume food or drink, a glucagon injection may be necessary. Glucagon is a hormone that stimulates the liver to release stored glucose into the bloodstream. Family members or caregivers should be trained on how to administer glucagon in emergencies.
Preventing Hypoglycemia in Diabetes
Preventing hypoglycemia is critical for individuals with diabetes, especially those taking insulin or other glucose-lowering medications. Key preventive strategies include:
- Frequent Blood Glucose Monitoring: Monitoring blood glucose levels multiple times a day helps individuals stay aware of their current blood sugar status and take preventive action when levels start to drop.
- Balanced Diet and Regular Meals: Consistently consuming meals rich in complex carbohydrates and protein helps to stabilize blood sugar levels throughout the day. Avoid skipping meals and ensure that snacks are available if meals are delayed.
- Medication Management: Adjusting medication doses based on activity levels, food intake, and blood sugar readings is essential. Healthcare providers can assist in making necessary adjustments to prevent hypoglycemia.
- Exercise Planning: People with diabetes should plan their exercise routines carefully, taking into account their medication and food intake. Checking blood sugar before and after exercise and adjusting insulin or carbohydrate intake accordingly can prevent hypoglycemia.
- Limit Alcohol: As mentioned earlier, alcohol can lower blood sugar levels, especially when consumed without food. Individuals with diabetes should limit alcohol intake and ensure they eat when drinking.
When to Seek Medical Help
While mild episodes of hypoglycemia can often be managed at home, certain situations require medical attention. These include:
- Frequent Hypoglycemia: If low blood sugar levels occur frequently, it may be a sign that diabetes management needs adjustment. A healthcare provider can help review medications, diet, and lifestyle habits to reduce the risk of hypoglycemia.
- Severe Hypoglycemia: If someone experiences severe hypoglycemia leading to loss of consciousness, seizures, or an inability to manage the episode independently, they should seek emergency medical care. In these cases, a glucagon injection or intravenous glucose may be administered in a hospital setting.
Conclusion
While hypoglycemia is not a direct indicator of diabetes, it can be a sign of poorly managed diabetes, particularly in individuals taking insulin or glucose-lowering medications. Understanding the causes, symptoms, and prevention strategies is key to managing hypoglycemia effectively and ensuring stable blood sugar levels. Through proper medication management, balanced diet, and lifestyle adjustments, individuals with diabetes can reduce the risk of both hyperglycemia and hypoglycemia.
For more detailed information on managing diabetes, visit Diabetes.org and NIDDK, which offer comprehensive guides on the condition and treatment options.
By incorporating thorough research and applying the best practices, we aim to create content that is not only informative but also actionable for individuals navigating the complexities of diabetes and hypoglycemia. This guide provides the necessary insights for both healthcare professionals and patients managing their conditions.